Inhaltsverzeichnis
What is artificial intelligence
Artificial intelligence (abbreviation AI) is a branch of computer science that deals with the Automation of intelligent behaviour and machine learning deals with. In practice, AI is often used as a collective term for algorithmic systems that can solve specific tasks. The term artificial intelligence is generally used very broadly. The reason for this is that in the absence of a precise definition of intelligence, it cannot be clearly delimited.
Very often, artificial intelligence and machine learning are used synonymously. Strictly speaking, however, machine learning is a subarea of artificial intelligence in which an artificial system learns rules from numerous examples that it can subsequently generalise. Put simply, machine learning is the creation of a computer-controlled system that finds solutions to a problem. Learn to solve a recurring problem yourself can.
Possibilities of AI in medicine
Medical technology
Medical technology is one of the subsectors in which AI in medicine has already been used for some time and in is used in a variety of ways. A number of medical technology systems based on artificial intelligence have already received approval as medical devices in the USA and Europe. The use of AI in medical technology is possible in all phases of patient care. It begins in prevention and extends through screening, diagnosis, therapy planning and therapy to aftercare and rehabilitation.
Very often, systems based on artificial intelligence are used in the Area of prevention used, for example, in the form of health assistants that encourage people to lead healthier lifestyles. A very broad area of application for AI in medical technology is diagnostic imaging. AI-based systems are nowadays very good at identifying conspicuous image areas. In cancer radiotherapy, AI systems can suggest optimised radiation plans. In the field of cardiology, artificial intelligence systems are already able to detect cardiac arrhythmias based on long-term ECGs. In anaesthesia, intelligent systems can be used to detect life-threatening conditions at an early stage. In the field of dermatology, AI systems are used to detect malignant skin lesions. In neurology, artificial intelligence is used to predict epileptic seizures. And in endocrinology, diabetes patients can be advised on their therapy by machine learning systems.
Medical diagnostics
The accurate diagnosis of diseases is one of the most difficult questions in medicine in many specialties. It usually requires not only lengthy training but also years of experience on the part of a doctor. In his diagnosis, a doctor not infrequently relies on the wealth of experience he has acquired in the course of his career.
This is where the advantages of artificial intelligence come into play. Powerful computer systems, in combination with large databases, can be a great help in diagnosing many diseases. The progress made in machine learning in recent years allows AI to be used promisingly in more and more areas of medical diagnostics.
Similar to an experienced doctor, machine learning algorithms can learn independently, recognise certain patterns of disease. In contrast to a doctor who has or will only see a few hundred or thousand cases of a disease in his lifetime, AI systems can be fed with thousands and thousands of data and on this basis train and continuously improve their diagnostic ability.
Against this background, AI in medicine can be used particularly well in those areas where diagnostic information is already available in large numbers in digital form. This is the case, for example, with CT scans, electrocardiograms, skin images and heart MRI scans. For example, AI systems are already able to diagnose lung cancer or strokes on the basis of CT scans, classify skin lesions on the basis of skin images or determine the risk of sudden cardiac death or other heart disease on the basis of electrocardiograms and heart MRI images.
In the largest internationally conducted PwC "Sherlock in Health" study for automated skin cancer detection, 511 medical professionals from 63 countries were compared with 139 computer algorithms. The objective was to diagnose skin cancer based on dermatoscopic images of the seven most common pigmented skin lesions. In the study, the computer algorithms performed significantly better than the medical experts. Even average algorithms performed similarly well or even better. Perform better than human doctors.
These and many other recent studies give hope that the use of AI in medicine will lead to great advances in the quality and speed of diagnoses in the future. A computer algorithm is not only faster than a human, it is also cheaper and can be used regardless of location. This will enable countries with underdeveloped health systems in particular to participate in scientific findings in the future, which could hardly or not at all be applied in practice there until now.
Despite all the advances in computer technology, hopes regarding the use of artificial intelligence in medical diagnostics should not be exaggerated. It is still rather unlikely that AI will replace doctors on a broad front in the coming years. Rather, it will lead to a Symbiosis of man and technology in diagnosis of diseases. In future, doctors will be increasingly supported in their diagnosis by computer systems. However, a prerequisite for this is that doctors are able to understand the basis on which the computer algorithms have arrived at a certain assessment. Only in this way can people correct any misjudgements made by machines and further improve their algorithms.
Production of medicines
One of the biggest and most promising areas of application for AI in medicine is the production of medicines. The development of drugs is not only a time-consuming but also a very costly undertaking. However, since the process of drug development consists of very many individual analytical steps in which work is done with a large database, there is a need for AI. Machine Learning systems are virtually predestined to be used in drug research.
Pharmaceutical practice shows that artificial intelligence can be used successfully in all stages of drug development. This begins in the identification of the so-called intervention targets. The basis for the development of a drug is the understanding of the biological origin of a disease and its resistance mechanisms. Provided this understanding is given, targets (usually proteins) can be identified to treat the disease. The now large Availability of high-throughput screening methodswhere high-throughput biochemical, genetic and pharmacological tests are performed on many thousands of substances, is an excellent database for the use of machine learning systems to identify target proteins.
In stage 2 of drug development, a suitable compound must be found that interacts with the identified target molecule in the desired way. Also in this stage, an enormous number of potential compounds have to be investigated for their effect and likewise their side effects. Due to their learning ability, machine learning systems are able to screen and assess millions of target molecules and identify better and better molecules with greater efficacy and fewer side effects based on a trial and error process. This stage in particular holds enormous potential for time and financial savings in the development of medicines.
The implementation of clinical trials (stage 3 of drug development) can also be massively accelerated through the use of AI. In most clinical trials, the identification of suitable test subjects is still a problem that in practice leads to delays in the approval of drugs. Machine learning can speed up the implementation of clinical trials by automatically identifying suitable test subjects and ensuring that the groups of study participants are put together in a sensible way.
Last but not least, AI can also assist in the fourth stage of drug development, which involves finding biomarkers to diagnose a disease. Biomarkers are molecules in body fluids that can be used to clearly identify diseases. The process of identifying suitable biomarkers for a particular disease is often time-consuming and costly. AI can provide valuable services in classifying molecules into suitable and unsuitable biomarkers.
Personalised treatment
Every person reacts differently to the use of medicines and other therapeutic options. Personalised treatment of patients could be one of the greatest potentials in many areas of medicine for improving individual therapies and ultimately for Increasing life expectancy and quality of life of the people affected. Especially in complex therapies, such as cancer, personalised treatment offers enormous potential.
Currently, however, determining the factors for personalised treatment is often not feasible due to technical or financial limitations. The use of AI in medicine can reduce these limitations in the future. AI systems can use their analytical and learning capabilities to find out which factors determine whether a patient responds well or poorly to a particular therapy. By comparing thousands of patient records, AI systems are able to identify patterns in personalised treatment, if any, and thus help doctors design an individualised treatment plan.
Improving gene editing
Gene editing is the insertion, deletion or replacement of gene sequences in DNA that lead to a change in the way the organism functions. The greatest leap in development in this field took place in 2012 with the Discovery of CRISPR took place. Scientists discovered that certain bacteria use gene editing as a defence mechanism and realised that they could apply this ability to selectively edit DNA.
CRISPR turned out to be much faster, easier and cheaper than other gene editing approaches. But the method is not without pitfalls. One of the main difficulties is identifying those gene segments with the least unintended side effects. Machine learning systems can be very effective in supporting scientific research on this issue and can greatly speed up the testing of gene editing for side effects.
Psychology
Psychology is the discipline in which AI in medicine is the least possible use be certified. According to a survey, more than 80 per cent of psychologists consider it unlikely that an artificial intelligence will ever be able to provide adequate psychological or psychiatric treatment. AI systems can develop certain diagnostic and prognostic skills based on data, but they cannot learn professional skills that are essential for the delivery of psychological or psychotherapeutic treatment.
Cancer research
Cancer is one of the specialties where doctors expect the greatest support from the use of AI in medicine. Not only are cancers particularly widespread in the population, they also produce very large amounts of data as part of diagnosis and therapy. In the case of cancer patients, X-ray images, tissue samples, tumour markers in the blood as well as genetic information must be correctly processed and interpreted. A performance that requires a lot of work or computing power. AI systems are already able to support oncologists in the evaluation of medical images, gene sequences and tissue samples. Their high computing power and learning ability make them an ideal auxiliary tool in the detection and treatment of cancer.
The quality and reliability of AI systems in the fight against cancer has already been proven in several studies. In a study with MRI images, an AI system was able to recognise areas of the brain suspected of tumours just as reliably as experienced doctors. And in another study based on 2,000 MRI images, an AI system was even better able than doctors to assess the patients' response to therapy.
In everyday clinical practice, AI systems currently still play a minor role in the treatment of cancer. This is due to several aspects. Firstly, due to its severity, cancer is a very emotional matter that can only be assessed by humans for the time being. Computers do not (yet) have empathy and therefore cannot put themselves in the shoes of cancer patients. On the other hand, AI systems must be trained for broad use with data from different clinics. This data exchange is often not yet given in practice.
Despite these difficulties, research into further applications of AI in cancer is going ahead at full speed in many areas. With the help of artificial intelligence, doctors should be able to create an exact profile of cancer cells in the near future. On this basis, the most effective drugs and forms of therapy can then be defined for each individual patient.
Triage bots
Triage bots are still a very young field of application of AI in medicine. A triage bot is an intelligent chatbot that can give people an initial assessment (triage) of a possible disease based on certain data they provide.
For private individuals, triage bots can be a great practical help. Most people are familiar with the situation of searching the internet for symptoms of an illness they or a family member are currently facing. In most cases, however, the internet is a very poor source for self-diagnosis. In future, triage bots are to provide a remedy.
Based on the symptoms a person provides to the triage bot, the bot's underlying AI system can ask the person further questions necessary to more accurately diagnose the possible condition. At the end of this process, the triage bot can provide the person with an initial assessment of their condition and make a recommendation as to whether or not a visit to the doctor or even a trip to the nearest hospital emergency room is necessary.
Triage bots are one of the most controversial applications of AI in medicine. While some experts see them as a completely unqualified replacement for doctors, others are of the opinion that the bots can be a valuable aid for people who do not have access to a doctor at the moment.
Covid-19
Artificial intelligence has already proven to be an important tool in the fight against the coronavirus pandemic. Machine learning systems are used worldwide to identify risk groups as quickly as possible. This involves not only determining how high a person's risk of contracting COVID-19 is, but also assessing how high the risk of a severe course of the disease is.
Another sub-area in which AI can be used against the spread of the coronavirus is patient diagnosis. Due to the huge amounts of data generated in this process, machine learning systems are ideally suited to detect people with viral symptoms at an early stage. For example, AI systems can be used to determine whether people have a fever or not via facial recognition.
Machine learning systems are an equally powerful tool in the identification of existing drugs with more or less efficacy against coronavirus. With the help of Language Processing millions of scientific articles can be searched and biomedical networks can be created from them that meaningfully correlate drugs and proteins. Machine learning systems can also predict the interactions between drugs and viral proteins.
We, Alexander Thamm GmbH, are also working together with the Ludwig Maximilian University of Munich on Early Warningystems for new corona infections. The aim is to predict daily infection figures so that regional health authorities can take appropriate measures against a further spread of the virus at an early stage or relax existing restrictions. The method will also optimise the data-based information flow for authorities and could also be used in other medical areas in the future.
And last but not least, AI systems are also used to identify the hosts of viruses in nature and predict the next virus pandemic on this basis. With the help of machine learning systems, those virus strains that have a higher potential to spread to humans can be identified more quickly.

Free white paper
We have prepared and summarised all the important contents for you. The white paper contains the following points:
- Explanation of basic terms
- Entry AI in medicine
- Areas of application
- Use Cases
- The state of research
Prerequisites for the application of AI in medicine
The most important prerequisite for the application of AI in medicine is the Data availability. All artificial intelligence systems are based on the analysis of data sets. Basically, the larger the underlying data set, the greater the AI system's ability to analyse and probability of success.
In practice, this means that all parties involved in the health system (general practitioners, specialists, clinics, health insurance companies, etc.) must digitise their existing data in a first step. In a second step, uniform data formats or standardised interfaces must be used to ensure that the data can be exchanged smoothly between all parties. For a meaningful and large-scale use of AI in medicine, data must be available as comprehensively and structured as possible. The data sovereignty of individual parties or even data islands that have no data exchange with other participants mean that the evaluable population is too small for the meaningful use of AI in medicine.
Besides the Quality and compatibility of data However, in connection with the use of AI in medicine, a number of ethical, social and legal issues must also be clarified. Central among the prerequisites for the application of AI in medicine is the question of adequate data protection. Artificial intelligence should be used as far as possible on the basis of anonymised patient data. The danger is too great that data will be misused and misappropriated.
Framework conditions
The use of AI in medicine requires a network of framework conditions in different areas. As already touched on in the last section, the following are tangential artificial intelligence not only purely medical, but also ethical, social and legal issues. These must be adequately discussed with all parties involved before the use of AI in medicine, and must be addressed in the framework of a Overall social consensus in laws and guidelines be poured.
In order to create the necessary framework conditions for the use of AI in medicine, the Federal Ministry of Education and Research has launched the so-called Medical Informatics Initiative. The initiative is intended to create the conditions so that in future every doctor, every patient and every researcher will have access to the information they need. Within the framework of the initiative, all university hospitals in Germany are working together with research institutions, health insurance companies, businesses and patient representatives to develop the framework conditions so that in future findings from research can be made directly accessible to patients.
To achieve this goal, work is being done on linking research and care data across locations. At the same time, innovative IT solutions are to be developed to exploit all the possibilities of digital services in the health sector.
The digital twin in medicine
A digital twin is the virtual image of a patient. In the future, a digital twin should make it easier to administer medicines and other medical products to patients. to test safely on patients. The digital twin is, if you will, one of the essential foundations for models of personalised medicine. The vision of doctors and scientists goes so far that when a patient visits a hospital in the future, the digital twin is already on site. The twin provides the hospital with all previous examination results, information about previous illnesses and operations, as well as genetic data, so that doctors can get a full picture of the patient and his or her course of illness. During diagnosis and therapy, the information from the digital twin is compared with data models of the clinical picture to ensure the most individual and effective therapy possible.
However, the great advantage of risk-free testing of medicines or medical devices and the provision of information in the health care system are still Many unresolved legal issues against. If the digital twin includes information about a specific patient, the right to informational self-determination is given. Personal data related to health are particularly strongly protected by the General Data Protection Regulation. As a rule, the patient's consent to the transfer of his or her personal data is required.
Status today / State of research
Despite all the spectacular success stories of recent years, the use of AI in medicine is still in its infancy. The pioneer in the application of artificial intelligence in medicine is the field of Radiology. CT, MRI and X-ray images are particularly suitable for analysing through machine learning systems. In addition to the automated skin cancer study presented in the section on medical diagnostics, a number of other comparative studies have been conducted in recent years.
In a study conducted by Stanford University in the USA, it was shown that a Algorithm 14 diseases of the lungs and chest better than radiologists. At the University of Yokohama in Japan, doctors have Endoscopic video recordings of colonoscopies evaluated with the help of AI systems and malignant polyps were detected almost as reliably as after a pathological examination.
Some machine learning systems are already in daily use around the world. At Massachusetts General Hospital in Boston, artificial intelligence is being used in the Analysis of X-rays of the breast used. And in Germany, the melanoma diagnosis system of the University of Heidelberg is in use in dozens of medical practices.
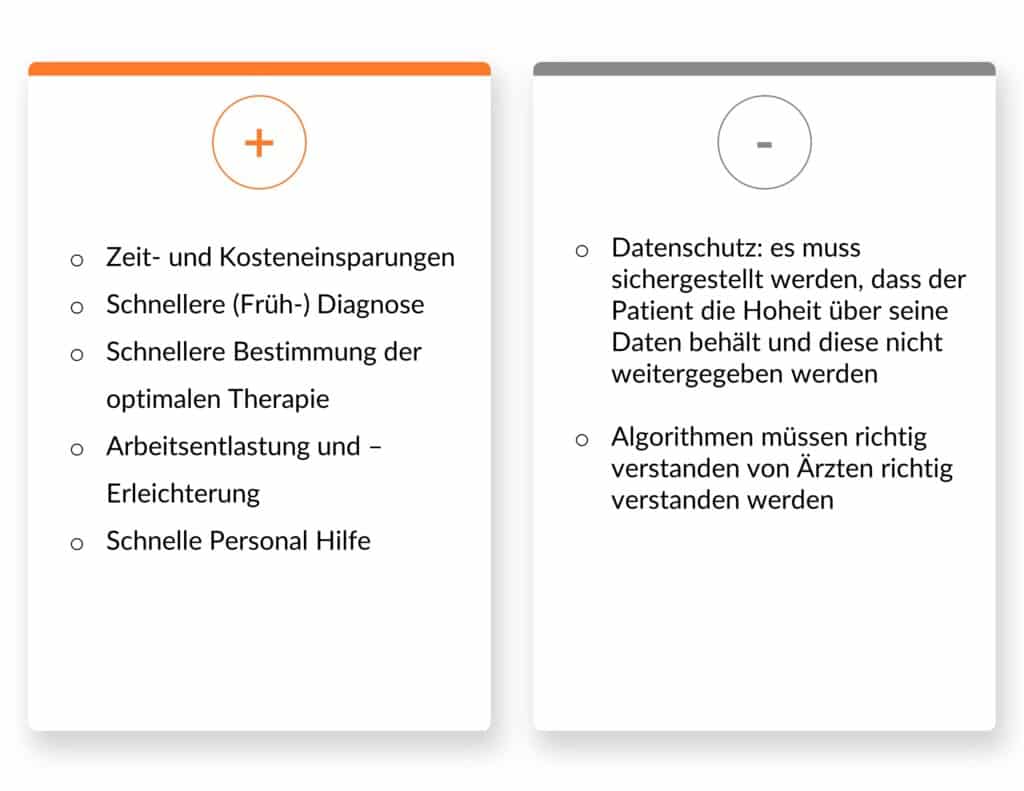
The advantages
As outlined in the previous sections, the use of AI in medicine brings a variety of benefits. First and foremost, AI systems can bring about significant time and cost savings in many medical disciplines and especially in drug development. The analysis of large and complex amounts of data can ensure faster (early) diagnosis of diseases. In addition, AI systems can be used very meaningfully in the selection of the optimal therapy method.
All in all, AI systems in medicine represent a Reducing the workload and facilitating the work of doctors This means that doctors can focus their scarce time on those issues where computer-based systems cannot yet provide support. As a result, doctors can focus their scarce time on those issues where computer-based systems cannot yet provide support. And last but not least, AI in medicine has great potential for countries or regions where the healthcare system is not particularly well developed. Particularly in areas with a low density of doctors, the use of AI in medicine can help to relieve doctors as much as possible of the burden of diagnosis and therapy from AI systems.
The disadvantages
The two big Risks and challenges of AI in medicine are the Data protection and the Understanding the algorithms. Data protection is primarily a legal issue, where it must be ensured that patients still retain sovereignty over their health-related data. The challenge in terms of understanding algorithms is that scientists and doctors should not blindly trust machine learning systems and diagnosis and therapy should not be delivered by a "black box" AI system. In Europe, for example, there are still no guidelines for the approval of adaptive diagnostic systems. The USA is already a step ahead in this regard.
Conclusion
Medicine is one of the largest and most promising application areas for artificial intelligence. The use of AI in medicine can help diagnose diseases more accurately, develop medicines faster, edit genes with pinpoint accuracy, personalise therapies and provide patients with self-diagnosis tools. The application of AI in medicine has already led to some high-profile successes in recent years. Nevertheless, as in all areas of application, artificial intelligence is still in its infancy in medicine. Due to the constantly growing volume of data and increasingly powerful algorithms, AI systems will be able to take over further tasks in medicine in the near future and contribute to a more efficient, cost-effective and, above all, more intelligent healthcare system.






0 Kommentare